Your battle, our fight to win with you.
There are two components of breast cancer surgery:
- The first deals with removing the breast tumor; this can be done either by removing the entire breast (mastectomy) or removing just the tumor and a small amount of surrounding normal breast tissue (breast-conserving surgery or lumpectomy). Some women with early stage breast cancer who are candidates for lumpectomy may also benefit from Intraoperative Radiation Therapy (IORT). IORT can spare some women weeks of radiation therapy.
- The second part involves removing the lymph nodes. This is necessary to find out whether the tumor has spread to the lymph nodes. Ideally, these two components (breast and lymph node surgery) are performed at the same time.
A mastectomy is the surgical removal of the entire breast. There are several different types of mastectomies:
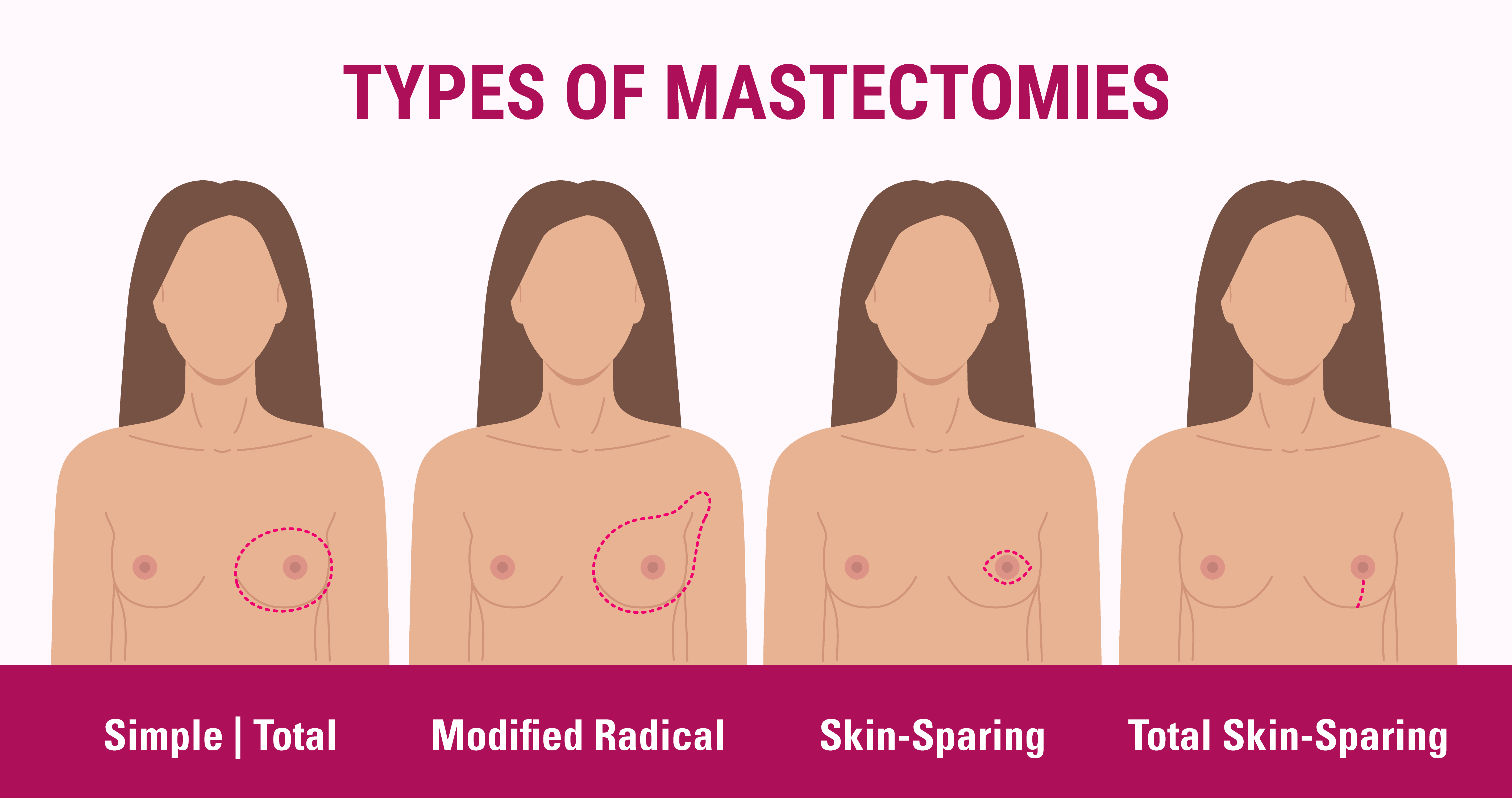
A mastectomy is the surgical removal of the entire breast. There are several different types of mastectomies:
- Simple Mastectomy: A “simple mastectomy” removes the breast, nipple and areola (the tan or brown-colored area surrounding the nipple) but it does not remove the axillary (armpit) lymph nodes.
- Modified Radical Mastectomy: A modified radical mastectomy is the removal of the entire breast, the lining over the chest muscle and some axillary lymph nodes. When the axillary lymph nodes are removed the surgeon may place a soft, plastic drain in the wound to drain the fluid that typically collects there. The drain remains in place when the patient goes home from the hospital. Before leaving the hospital, the patient is taught how to empty and take care of the drains. These drains are typically removed at the first post-operative check-up.
- Skin-Sparing Mastectomy: Skin-sparing mastectomy is a technique that preserves as much skin as possible when performing a mastectomy. This is done to help the plastic or reconstructive surgeon provide the best cosmetic result during breast reconstruction. However, if the surgeon believes there is an area of skin that is involved with the tumor, this portion of the skin will be removed along with the tumor.
- Total Skin-Sparing Mastectomy: Total skin-sparing mastectomy is similar to the skin-sparing mastectomy, but the nipple and areola tissue are left along with the skin. Because the ducts, which can contain tumor cells, drain to the nipple, there are some restrictions/limitations for this approach.
Breast-conserving surgery (BCS) involves a lumpectomy (the surgical removal of a tumor and a margin of normal tissue) followed by radiation therapy to the remaining breast tissue. The goal is to excise the tumor while maintaining a cosmetically-acceptable breast. If the breast is very small and the tumor is large, BCS may not be an option because the surgery could create a cosmetically unacceptable breast. Additionally, patients who are pregnant may not be amenable to this technique because the radiation therapy might be harmful to the developing fetus.
Other terms that describe the removal of the tumor and a margin of normal breast include, partial mastectomy, segmental mastectomy and quadrantectomy. Because all of these techniques leave some breast tissue behind, they are considered breast conserving.
An important aspect of BCS is assuring the margin of normal tissue surrounding the tumor is free of cancer cells. Once the tumor is removed, the pathologist will evaluate the margins. If the margins are positive (cancer cells extending to the edge of the resected tissue), the patient will need to have a re-excision to remove more normal tissue from the tumor bed area to assure that all cancer cells have been removed.
INTRABEAM® IORT technology, available at St. Luke’s Anderson Campus, spares some women with early-stage breast cancer weeks of radiation therapy. Fewer than 50 sites nationwide offer this advanced radiation therapy.
Breast cancer surgery has two main goals – to remove the cancer via a mastectomy or lumpectomy and to determine if any cancer cells have spread to the lymph nodes. Surgery is recommended for patients with invasive breast cancers. Breast cancers like Ductal carcinoma in situ (DCIS) that are non-invasive cannot spread beyond the ducts and lobules. Therefore, these patients do not need their lymph nodes evaluated. One exception to this concept is if the surgeon suspects that invasive cancer will be found when the entire tumor is removed.
Two operations are used to evaluate the lymph nodes.
When too many lymph nodes are removed, many patients develop lymphedema (arm-swelling). To minimize the risk of lymphedema and still provide an accurate assessment of the lymph nodes, sentinel lymph node biopsy can be done.
The sentinel lymph node (SLN) is the first lymph node to receive drainage from around the tumor and is typically the first to be invaded by cancer cells. The SLN is tested for cancer at the time of surgery. If there is no cancer in the SLN, it is unlikely that it has spread to other lymph nodes and so they are left alone. If cancer is in the SLN, the standard operation (axillary dissection) is performed. Sentinel lymph node surgery has fewer complications than axillary node dissection, but the physicians performing the procedure must have special training.
Technology is available to evaluate the genetic profile of individual tumors. St. Luke’s uses these to help determine if chemotherapy should be given as an adjuvant therapy. Today, two main tests are used — OncotypeDX® and MammaPrint®. OncotypeDX® uses 21 genes to estimate the risk of a tumor recurrence. MammaPrint®, an FDA-cleared gene expression profile test, provides information based on 70 genes about tumor biology and actively identifies a woman's risk for recurrence.
The 70-gene genomic profile can provide prognostic information in both ER-positive and ER-negative early-stage, node-negative breast cancer. However, this test requires that the tissue be appropriately preserved at the biopsy procedure or at the time of surgery. Therefore, having this test done should be discussed with the surgeon prior to surgery.
St. Luke’s Hospital is one of only a few hospitals in Pennsylvania and was one of the first in the state to use MarginMarker® to color-code cancerous breast tissue immediately after surgical removal to see if the entire cancer was removed during the procedure. Using six different inks, the operating surgeon color-codes the entire excised breast tissue specimen to show exactly how the tissue was positioned or oriented in the body.
St. Luke’s fellowship-trained surgical oncologists and most general surgeons performing breast cancer surgery at St. Luke’s Hospital have used this innovative device since 2008. It allows for higher precision and greater accuracy for surgeons, radiologists and pathologists involved in the patient’s care, and it helps improve outcomes following breast cancer surgery.
This is a procedure to restore the natural appearance of the breast and is frequently performed after partial or total mastectomy. Patients treated with a lumpectomy procedure often do not require reconstruction. Some patients may choose delay reconstruction of the breast until a later date. Consultation with a board-certified plastic surgeon, experienced in breast reconstruction is warranted in all of these instances.
Your health matters: find the right gynecologist.
Navigating your health journey can feel overwhelming, but finding a compassionate gynecologist shouldn’t be. Whether you’re looking for routine check-ups, specialized breast health services, or support through life’s changes, we’re here to help you connect with a dedicated provider who understands your needs.