Pocono Resort GM Recovers from Stroke with SLUHN Help
January 17, 2024

Pocono Resort GM Recovers from Stroke with Help of St. Luke’s
Don Pleau can recall with disturbing clarity the moment he realized something was seriously wrong. It was on a November evening five years ago when he was awakened with an intense wave of nausea. Unable to find his balance, the then-54-year-old stumbled to the bathroom, got back to his bed and woke up the next morning to get ready for his demanding role as general manager of one of the country’s largest indoor waterparks, resort and convention centers. He drove on a series of winding Pocono roads to drop off his dog at the pet groomers and then went into the office.
Throughout the day, he said, “I felt worse and worse. I thought maybe it was something I’d eaten. At the end of the day, I got myself back to my car, picked up the dog, went home and went to bed.” It was only the following day, after his wife insisted they go to the emergency room at the St. Luke’s Monroe Campus, did the couple learn that Pleau had suffered a stroke roughly 36 hours earlier and would be facing a grueling journey to a complete recovery.
Pleau was fortunate to be able to access St. Luke’s stroke care, a national leader in the field that has earned top honors from the American Heart Association, the American Stroke Association, Healthgrades and the Joint Commission. Immediately upon reaching the St. Luke’s ER, one of Pleau’s nurses recognized the signs of a stroke. With blurring speed, he found himself in the ICU and undergoing hourly neurological tests. Further testing revealed the cause of his stroke: a fully occluded artery on one side of the cerebrum and a partial occlusion on the other, with only 25 percent of blood flow reaching his brain.
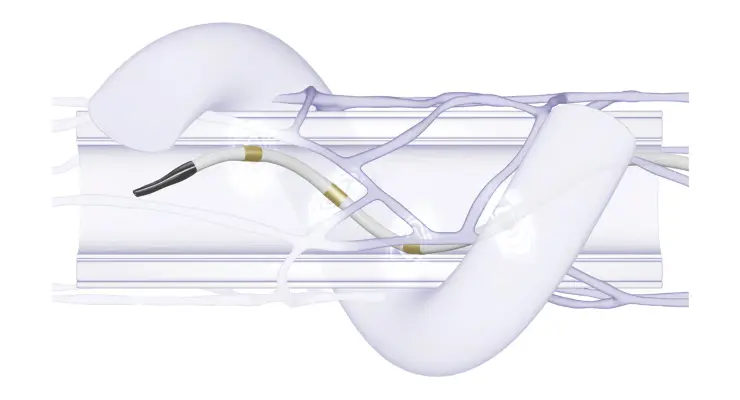
Pleau was transferred to the St. Luke’s Bethlehem Campus and was placed under the care of Neurointerventional Radiologist Dr. Martin Oselkin, who performed a delicate, multi-hour arterial angioplasty and stenting to restore blood flow to the brain.
“I’ll never forget how caring he was with me,” Pleau recalls. “He came in and sat down and took the time to explain exactly what the issue was and how we were going to approach the problem. I feel really fortunate that I had one of the best doctors in the country, supported by an unbelievable, highly effective team of physician assistants and nurses. They really care about their patients, and it was apparent in every level of care.”
Oselkin said that by coordinating emergency medical services and the emergency room network with advanced imaging and communications platforms, “we are able to quickly diagnose patients suffering from a stroke and get them the care they urgently need.”
“The old adage in our field is ‘time is brain,’ because 1.9 million brain cells are lost with each minute that passes when suffering from a stroke, which is a blood clot in the brain. Once we identify the problem, our expertly trained stroke teams are either able to remove the clot with minimally invasive surgical techniques or administer special medication to help dissolve the clot. Therefore, the quicker we can diagnose you and the quicker we can treat you, the better your outcome will be.”
The initial, emergency-level response is only part of the journey for the stroke patient, Oselkin said. Immediate treatment is followed by comprehensive testing to determine the cause and treatment. “At this time, we also begin various therapies to aid in recovery. We have dedicated nursing floors for stroke patients and the nurses on those units have additional training in stroke care and prevention,” he said.
“The team at our Physical Therapy at St. Luke’s office in Blakeslee provide exemplary and compassionate interdisciplinary care.” David Kozich, PT, DPT was Don’s Physical Therapist at the Blakeslee office.
A remarkable recovery
Pleau’s recovery – although not easy – has been remarkable, according to Oselkin. “He was and still is a model patient,” Oselkin said. “He did not look at his stroke as a setback or a loss but rather an opportunity for him to adopt a healthier lifestyle and to commit himself to the challenge of physical therapy in order to regain his prior abilities and to prevent his stroke from recurring.”
This past November, Pleau joined the roughly 25 percent of stroke sufferers to survive five years. With regular check-ups revealing no issues, Pleau continues to challenge himself physically and mentally. He works on word and math puzzles, does strength training, taught himself new skills, walks everywhere he can to regain a sense of balance and continues to focus on recovery with a single-minded determination that impresses even his physicians.
Comparing him to an elite athlete in training for the Olympics, Oselkin said Pleau rose to the challenge, “with a dedication I wish all patients could have.”
Pleau’s advice for other stroke sufferers: “Number one, listen to your doctors and your caregivers. If they tell you go to physical therapy, go to physical therapy. Number two, attack the stroke in a healthy, methodical way. Pay attention to those benchmarks, like where you should be in the first seven days, in the first 14 days, and then build on that. Change your diet and your health habits. Stroke recovery is a marathon, not a sprint.”
And, he adds, consider emotional therapy – advice he failed to take himself. “I fought against massive depression,” he said. “It was as if depression sat on my shoulder the entire time and whispered in my ear. But I kept myself busy, kept working. I’d advise anyone going through this to get the help you need. It’s one of the most difficult situations you’ll ever go through. And if you’re serious about recovering, you can do it. You can get your life back.”
BE FAST: Learn to recognize the symptoms of a stroke
Don Pleau’s story stands as a testament to how timely and effective stroke treatment, combined with self-care and determination, can result in optimal recovery. Dr. Martin Oselkin, a neurointerventional radiologist with the St. Luke’s, said that a stroke can affect anyone at any age, making it essential to recognize the following “BE FAST” warning signs and symptoms and to seek medical attention as soon as possible:
B – Balance: Is the person suddenly having trouble with balance or coordination?
E – Eyes: Is the person experiencing suddenly blurred or double vision or a sudden loss of vision in one or both eyes without pain?
F - Face Drooping: Does one side of the face droop or is it numb? Ask the person to smile.
A- Arm Weakness: Is one arm weak or numb? Ask the person to raise both arms. Does one arm drift downward?
S - Speech Difficulty: Is speech slurred, are they unable to speak or are they hard to understand? Ask the person to repeat a simple sentence like, “The sky is blue.” Is the sentence repeated correctly?
T - Time to call 911: If the person shows any of these symptoms, even if the symptoms go away, call 911 and get them to the hospital immediately.
Read More NewsLatest News

December 20, 2024
Top Baby Names of 2024 at St. Luke's

December 19, 2024
Fitness Center Devotee Joel Rosenfeld
December 18, 2024